SUD Assessments
Substance Use (SU) Assessments Overview
The new HHSC Substance Use Disorder (SUD) Assessment performs some of the same calculations as the previous Substance Abuse (SA) Assessment, such as the client’s HHSC Priority Population and the Severity Score to identify areas to be addressed in the client’s Treatment or Service Plan.
The new SUD Assessment also provides these additional features:
- The Severity Score calculation results in the display of Mild, Moderate, or Severe for the DSM-5 diagnosis;
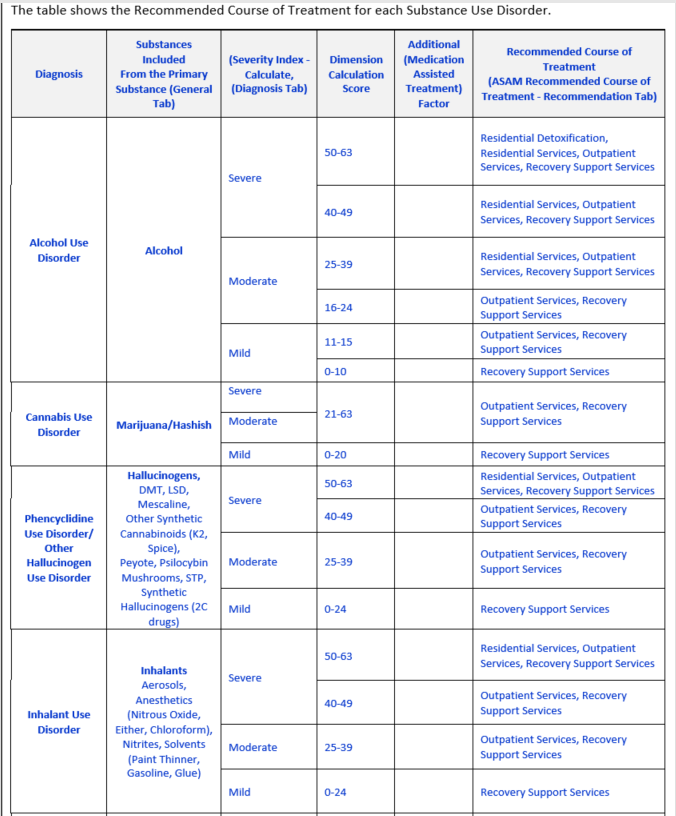
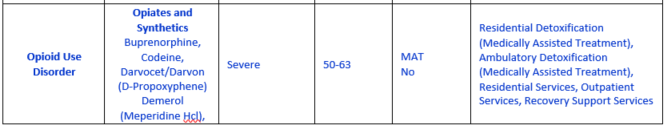
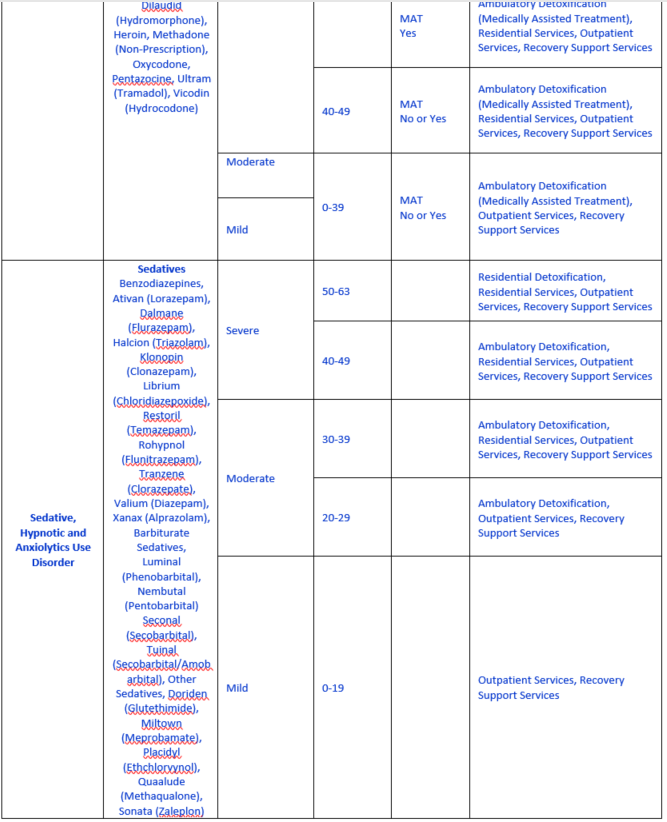
- The American Society of Addiction Medicine (ASAM) Recommended Course of Treatment is calculated;
- The American Society of Addiction Medicine (ASAM) Modifications to Treatment calculations is displayed on the Recommendations tab.
The SU Assessment questions are guides for counselors and interviewers, who may present the questions in whatever form will allow them to best communicate with their clients. We encourage counselors to use rapport building skills during the initial assessment. This will facilitate collection of the most accurate information for the important purpose of recommending a course of treatment for the client. And it will aid in the development of a treatment plan to assist the client in achieving his or her treatment goals.
The questions in the assessment are designed for adults and youth. There are some items in the Employment section and Family Social tab that will only display when the Client Profile indicates the person is 18 years old or older. All other items will display for all ages.
General Information about all Assessment Types
An assessment, more comprehensive than a screening, is a health professional’s review of an individual. The review consists of evaluation of a variety of domains including current and past functioning in the areas of mental health, substance use, risk of harm, physical health, education, employment, family, and socialization.
From the assessment, the clinician identifies the person’s problems, goals, strengths, and limitations; and then formulates a diagnosis. The assessment is the foundation for collaboration with the client on development of the plan for treatment and recovery. The strengths and limitations are used to individualize services in ways that increase their likelihood of being beneficial to the client.
CMBHS provides separate assessments for clients requesting substance use services vs. clients requesting mental health services.
When a clinician has entered all the required information into an assessment, CMBHS calculates and recommends a level of care. For substance use services clients, a list of problem statements is also generated that is used as the foundation for the treatment plan, providing a starting place for the collaborative treatment planning process.
Before You Start an Assessment
Your business entity must have a contract (or other approved written agreement) with HHSC to perform Substance Use Assessments and document them in CMBHS.
The CMBHS user must be assigned a role that permits documentation of Substance Use Disorder assessments. You must have the proper credentials and they must be accurately entered into your CMBHS account in order to be assigned those roles. Click here for a summary of Roles in CMBHS and each role's Read-Only or Read-Write Page Rights.
Some CMBHS roles permit the user to document assessments, but the user cannot put the assessment in Closed Complete status. Because of their limited credentials, they may only place the assessment in Ready for Review status. It must then be signed off by a clinician who can put the assessment in Closed Complete status.
The client must have, at minimum, a profile in CMBHS before an assessment can be documented.
Before you attempt to document an Assessment in CMBHS, make sure you are fully aware of how to use the Document Status and Save functions. Knowing how to use these functions will reduce the likelihood of losing information or making errors that cannot be corrected. For more information about Document Status, click here.
Verify that you have the correct client record by checking the client’s name and at least one other identifier before you begin to document.
The CMBHS Assessment is not a script from which the Clinician should ask the client questions word for word as they are written. Ask the questions using words the client will understand to ensure that the assessment results are meaningful.
Business Rules for Assessments
The questions and data fields that display in the CMBHS Assessment are determined according to the user’s program type (mental health or substance use) and location.
Questions about the client’s substance use, mental health and physical health are available as part of the assessment regardless of provider type or service location. This gives the assessing clinician the opportunity to document clinically relevant information without being limited by provider/business entity type.
You do not have to complete the entire assessment in a single session. Any time you need to stop, you may save the Assessment in Draft status and return to it at another time.
An Initial Assessment in Closed Complete status must be in the client’s record for the current episode of care before a Treatment Plan can be created for the client.
CMBHS will allow only one Initial Assessment to be created per episode of care. If there is already an Initial Assessment for the episode of care and the user attempts to create a second one, they will receive the following error message “An Initial Assessment in Closed Complete status already exists for this episode of care. An Update Assessment can be performed by selecting it from the menu.”
Use the following links to go directly to Help about Assessments:
Detoxification Service End Assessment
Detoxification Discharge Assessment
Detoxification Discharge Follow-up Assessment
General Information on Substance Use Assessments
Before You Start an SUD Assessment
Assessments are completed at the CMBHS location level. Not all assessment types are available at all locations, so be sure to confirm your location and the SUD Assessment type you need to complete for the client
Click here to view page rights of read-only or read-write corresponding to different CMBHS roles.
Before you document in a client record, confirm that you have the record for the correct client. Correcting errors in CMBHS can be time-consuming and can put confidential client data at risk.
An SU Assessment can be completed for a client without an Admission or begin service.
The Texas Administrative Code includes requirements for timely completion of SU Assessments. Your organization may have additional rules. Be sure to confirm the timelines that apply to the client’s payer to ensure that billing is not interrupted.
Substance Use Assessment Types
There are three Assessment types for Substance Use Services. Each of the three types has two to five versions to ensure that all client situations are accommodated.
Treatment and Intervention Assessments
- Includes Initial, Update, Service End, Discharge, and Follow-up types.
- The Initial Substance Use (SU) Assessment contains the total set of questions for all the assessments.
- Discharge SU assessments are accessed within the Discharge page.
- The SU Discharge Follow-up can be found on the Client Services Toolbar (left side of CMBHS) under the heading of Discharge. This document may only be accessed after the client has been discharged from services for a minimum of thirty days.
Case Management Assessments
- Includes an Initial and Update version but not a discharge or service end version.
- The Case Management Assessment contains a subset of questions from the SU Assessment that is helpful in understanding the needs of clients who will receive Case Management services.
- The Case Management Assessment does not include entry of a Diagnosis. Instead of identifying symptoms, it focuses on identifying the client’s needs for support.
- The Initial and Update Case Management Assessments are available for Substance Use Treatment and Intervention locations and can be found under the left side Assessment menu after an Open Case has been entered for the client and Saved in Closed Complete status.
- Click here for more information about Case Management Assessments.
Detoxification Assessments
- Includes an Initial, Update, Service End, Discharge and Discharge Follow-up type.
- The Detoxification Assessment is available at CMBHS detoxification services locations and can be found in the Client Services Toolbar's Assessment menu.
- The Detoxification Assessment has a subset of questions from the SU Assessment and there are specific questions to address withdrawal symptoms for people withdrawing from alcohol or opioids.
- This Assessment type is only available if there is a Service Begin for a Detoxification service/level of care.
- Service End Detoxification Assessment and Discharge Detoxification Assessment can be accessed only within the Service End and the Discharge pages.
- The Detoxification Assessment Follow-up is under the heading of Discharge on the left menu after the client is discharged from services for a minimum of ten days.
Accessing the Correct SU Assessment Type
The SU Assessments are accessed from the Client Services Toolbar on the left side of the page, under the Assessment menu item.
Only the assessment types appropriate for the CMBHS location type will display in the menu.
Each assessment type is addressed in CMBHS Help. The instructions for documenting each assessment address the unique and common items.
The following table show the assessment types available at different Substance Use locations.
|
CMBHS SU Location Type
|
Assessment Types Available |
Comments Instructions |
|
Prevention/Intervention Location Prevention Service |
None |
Client level data is not currently documented at CMBHS Prevention locations |
|
Prevention/Intervention Location
Intervention Service
|
Case Management Assessment SUD Treatment Assessment
|
|
|
SUD Treatment Location
|
SUD Treatment Assessment Case Management Assessment Detoxification Assessment |
|
|
Detoxification Location, which is an SUD Location
|
Detoxification Assessment SUD Treatment Assessment Case Management Assessment |
|
|
Recovery Support (RSS) Location
|
Assessment of Recovery Capital (RSS) |
Addressed in the Recovery Support (RSS) section of the CMBHS Help |
The SUD Assessment Questions and Data Fields
The SU Assessment questions/data fields are grouped by topic and displayed in a tab format.
Assessment questions/data fields may:
- display in blank and required or optional status;
- display in edit status;
- display in view only status;
- display a slightly modified version of the item;
- not display in that version of the assessment.
Many of the required data fields are part of the five calculations available in the Substance Use (SU) Assessment for treatment. The calculations are used in the Initial Assessment only. These are explained in greater detail in the Help for the Diagnosis tab and the Recommendation tab.
The questions in the SU Assessment are used by CMBHS to calculate the following:
- The Severity Score calculation results in the display of Mild, Moderate, or Severe for the diagnosis.
- The HHSC Priority Population calculation result is displayed on the Recommendation tab.
- The American Society of Addiction Medicine (ASAM) Recommended Course of Treatment calculation is displayed on the Recommendation tab.
- The American Society of Addiction Medicine (ASAM) Modifications to Treatment calculations is displayed on the Recommendation tab.
- Many of the optional fields, are used to identify areas that need to be addressed in the client’s Treatment/Service Plan.
The SUD Assessment Business Rules
Most of the business rules are the same for all the SUD Assessment types. When there are differences, they will be identified in this section of the CMBHS Help.
In CMBHS online, required data fields are indicated on each page with a red
asterisk *. Optional fields do not have an indicator.
In CMBHS Help, (Required), (Optional) and (Conditionally Required) fields are identified in parentheses after the question.
Some required fields in the Update, Service End, and Discharge Assessments will be prepopulated by CMBHS with the answers from the previous assessment, but the user can edit these fields.
Other required fields must be filled in for each new version of the assessment because they contain information used by HHSC to comply with federal
reporting requirements.
How to Document a Substance Use Disorder Assessment and Document Status
To successfully document a Substance Use Disorder Assessment in CMBHS, complete all the required data fields under each tab of the assessment and save the document in Closed Complete status. Click here for more information about document statuses.
Closed Complete is a final document status. Documents in Closed Complete status can usually not be deleted or reopened and edited but sometimes a new version of the document can be saved.
Ready for Review is not a final document status. Use Ready for Review when someone else will be reviewing the document and putting it in final status.
Draft status is a final status for a document. Use the Draft Document Status when you cannot complete the assessment in one sitting.
Closed Incomplete is a final status for a document. Only use Closed Incomplete status when the client is unavailable and will not become available. This status is a final status for a document.
Substance Use Treatment Assessment – Initial
The following tabs display at the top of your screen when you are ready to perform an Initial SUD Assessment.
- General
- Education & Employment
- Legal
- Physical Health
- Mental Health
- Family & Social
- Substance Use
- Diagnosis
- Recommendation
General Tab
The General tab of the assessment includes questions and prompts to assist the clinician in gathering information about why the client is presenting for services today, when and where the Assessment took place, the referral source, and other service providers that are working with the client.
The data fields and questions under the General tab are the same for all clients receiving substance use disorder (SUD) service types and of any age.
Assessment Information
Assessment Number (Generated by the CMBHS System)
- Each assessment completed for a client and documented in CMBHS has a unique assessment number generated by the system. It is view only and cannot be changed by the User.
Assessment Date (Required)
- The user records the date that the client was assessed. The system will default to the current day’s date.
- If the assessment occurred on some other date before the current date, the user can change this field to the correct date. A future date cannot be entered.
- If the assessment interview occurred on more than one day, enter the first date that the assessment interview began.
- The system requires a full date using either of the following two formats: mmddyyyy or mm/dd/yyyy. When you enter the date using the mmddyyyy format (eight numbers with no slashes), the system automatically reformats and displays the date as mm/dd/yyyy. You may type in the forward slashes yourself if you wish.
- CLICK IN the text box and TYPE IN the information.
Assessment Type (Generated by the CMBHS System)
- The system will auto-fill the Assessment Type (Initial, Update, Service End or Discharge).
- This is a view-only field and cannot be changed by users.
Contact Type (Required)
Document the contact type that best describes of how the Assessment interview was conducted with the client.
CLICK ON one of the options available:
- Face to Face
- Telehealth
- Telephone
Assessment Site (Required)
- Document the setting where the Assessment interview took place with the client.
- Information may have been obtained from the client or collaterals in several settings. Answer this question indicating where most of the contact with the client occurred.
- Select the assessment setting that best describes where the interview(s) took place.
CLICK on one of the items in the dropdown box:
|
Ambulance, Land |
Boarding Home |
|
Community IMD |
Community setting (Community Mental Health Center) |
|
Correctional Facility |
Custodial Care Facility |
|
Emergency Room |
General medical hospital |
|
Group Home |
Home |
|
Hospice |
Hospital |
|
Independent Laboratory |
Inpatient Hospital |
|
Inpatient Psychiatric Facility |
Jail |
|
Mobile |
Mobile/Extended/ Outreach |
|
Not Applicable |
Nursing facility |
|
Office/Clinic |
Other |
|
Outpatient Hospital |
Psychiatric Facility Partial Hospitalization |
|
Psychiatric Residential Treatment Center |
Residential Substance Abuse Treatment Facility |
|
School |
Service facility |
|
State Mental Health Facility |
State Mental Retardation Facility |
|
State funded community hospital |
State or Local Public Health Clinic |
Referral Source (Required)
Document the person or organization who referred the client for services.
CLICK on one of the referral source options:
|
Community Health Service |
Community Mental Health Services |
|
Court Services/DWI/DUI |
Department of Family Protective Services (Adult or Child Protective Services) |
|
Drug Court |
Family/Friend |
|
Hospital (Community) |
Hospital (State) |
|
Insurance/Employee Assistance Program |
Outreach, Screening, Assessment, and Referral (OSAR) |
|
Peer Support/Recovery Support |
Probation/Parole |
|
School |
Self (Client) |
|
Substance Use Disorder Prevention/Intervention/ Treatment |
Work/Employer |
|
Community Service Provider (local, state, federal) |
|
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
Comments (Optional)
- The user may enter comments in this box that relate to any of the the Assessment Information fields.
- Comments will be entered into the client’s health record and will be seen by those who have the authority to view this part of the record. Under some circumstances, this may include the client. Always consider the consequences of entering sensitive information, such as HIV status.
- CLICK in the text box and TYPE in the information.
Presenting Problem (Required)
- Document the reason the client presented for services using the client’s own words.
- CLICK in the text box and TYPE in the information.
In the past 30 days: Applicable to all questions below as indicated.
— What substances have you been using? (Required)
- Answer the following question about the primary drug that the client uses in the first cell of the table.
- Select the Primary Substance Used by the client from the dropdown list.
- You may select a specific drug or a group of drugs, based on how much information is available and whichever best describes the drug the client uses.
- To receive substance use services, the client must have one or more “primary drug used” documented. If no primary drug used is documented, the client does not qualify for substance use services.
— Primary, (Required) Secondary (Optional) and Tertiary (Optional)
- If the client uses one drug, select answers in the row labeled Primary. If the client does not use one drug, select None and the remainder of the items will not be required fields.
- If the client uses two drugs, fill in the fields on the Primary and Secondary rows.
- If the client uses three drugs, fill in the fields on the Primary, Secondary and Tertiary rows.
- If the client uses four or more drugs, fill in the fields on the Primary, Secondary and Tertiary rows and put information about the other drugs used by the client in the Comment text box
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
— Route of Administration (Required)
Select the answer choice that represents how the client gets the substance into his/her body.
If the client uses more than one route of administration, select the usual or most frequently used route of admission.
CLICK ON the blue arrow to the right of the dropdown list, CLICK ON your answer, and then move to the next cell.
If you select Other, document the Other route of administration used by the client in the comments text box.
The answer choices are:
- Oral
- Inhalation
- Injection
- Smoking
- Other
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
— Frequency of Use (Required)
Document how frequently the client uses this drug by selecting one of the answer choices from the dropdown list.
CLICK ON the blue arrow to display the answer choices. The answer choices for this question are:
- No use in past month
- 1-3 times in the past month
- 1-2 times in the past week
- 3-6 times in the last week
- Daily
— Age at First Use (Required)
What was the client’s age when they first used this drug?
For drugs other than alcohol, these fields identify the age at which the client first used the respective substance.
For alcohol, these fields record the age of first intoxication.
Enter the client's age when substances other than alcohol were first used.
— Secondary (Required if the client uses a second substance)
- If the client uses a secondary substance, select the Secondary Substance used by the client from the dropdown list.
- If you select a substance on the row in the table labeled Secondary, then all the fields in that row will be required fields.
- See the above instructions for Route of Administration, Frequency of Use, and Age at First Use.
- If the client does not use a secondary substance, you may leave these fields blank.
— Tertiary (Required if the client uses a third substance)
- If the client uses a third substance, select the Tertiary substance used by the client from the dropdown list.
- If you select a substance on the row in the table labeled Tertiary, then all the fields in that row will be required fields.
- See the above instructions for Route of Administration, Frequency of Use, and Age at First Use.
- If the client does not use a third substance, you may leave these fields blank.
In the past 30 days: What substances do you seek? (Conditionally Required)
- This field displays and is Required only on the condition that one or more drugs are listed in the table.
- Use this text field to document the drugs the client seeks, whether it is one of the drugs listed or another drug.
- Document substances that the client sought if the preferred substance was not available or accessible to the client.
- CLICK IN the text box and TYPE IN the information.
— In the past 30 days: How many days have you used? (Required)
- Answer this question and the question below.
— In the past 30 days: How many days have you not used? (Required)
- Answer this question and the question above.
- The sum of the answers cannot exceed 30.
- This text field refers to the days of use within the past 30 days of any misused medication, or misused legal or illegal mind-altering substances.
- CLICK IN the text box and TYPE IN a number.
Comments (Optional)
Add additional information about the client’s substance use in the available text box. This comments text box is optional.
CLICK IN the text box and TYPE IN the information.
Literacy, language or auditory barriers? (Required)
- Document language, literacy, or auditory barriers and issues that the client may have.
- CLICK IN the Yes or No radio button to answer.
Comments (Optional)
- Add additional information about the client’s need for accommodation in the treatment setting in the available text box.
Other Service Providers (Optional)
The clinician identifies who provides the client with services, treatment, supports, or guidance for their physical, mental, emotional, or spiritual health and who may continue providing these while the client is in treatment.
Documenting information about other service providers is Optional, however if you document a service provider, you must enter a Provider Name and Provider Type. The Phone Number is Optional.
- CLICK ON the New Service Provider button, and the the required data entry fields will display.
- CLICK ON the arrow to the right of the Provider Type box that displays “None Selected” and select the Provider Type that most closely describes the provider’s service type.
- Click IN the Provider Name field and type the name.
- If you have the Phone Number, add it.
- CLICK ON the Add button to add the information to the table or Cancel to start over again. If you click Cancel, you will lose any data you have entered.
- You may add as many service providers as needed.
CAUTION: If you need information from these service providers, you may need to obtain the client’s consent to contact the provider for either written or verbal information. Click here to go to Help for Consent to Release Information.
Provider Type, Other (Required)
- If you select Other, document the type of service provided in the Comments text box below the table.
- CLICK IN the text box and TYPE IN the information.
Provider Name (Required)
- Document the Provider’s name, and credentials if available.
- CLICK IN the text box and TYPE IN the information.
Phone (Optional)
- This text field is optional. CLICK IN the text box and TYPE IN the information.
Comments (Optional)
- Add comments about the other providers that are serving client or other related information in the text field.
Staff Info (Information)
Interviewer (Required)
- The name of the user who first created and started documenting this Assessment will display in this field as the default.
- If the name that displays is not that of the person who interviewed the client, the name must be changed to the person who interviewed the client.
- CLICK ON the dropdown list to search for the name of the person who interviewed the client.
- CLICK ON a name to select it.
Primary Counselor (Required)
- The system will display the name of the assigned primary counselor.
- If the client has not been assigned a primary counselor, no name will display.
Comments (Optional)
- Add comments in the available text box related to staff information.
Document Status (Required)
Select the appropriate document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date
This is the date the document status is assigned.
Education & Employment Tab
Users document information about the client’s education and employment in this tab.
Education Section
What is the highest grade in school you completed? (Required)
CLICK ON one of the options available that best represents the client’s answer.
- <6
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- Bachelor
- Master
- Certification
- Other
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab. This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
If you didn’t finish school, why did you leave? (Required)
- CLICK IN the text box and TYPE IN the information.
- Type in the text box a summary of the client’s response
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
In what grade OR at what age did you start using alcohol or drugs? (Required)
Document in this field the highest school grade completed by the client.
Select from the dropdown list the answer closest to the client’s.
Then CLICK ON the number that best represents the client’s answer.
Grade: (Required)
- None
- 2nd
- 3rd
- 4th
- 5th
- 6th
- 7th
- 8th
- 9th
- 10th
- 11th
- 12th
- College
- Other
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Enter the client’s age when substances other than alcohol were first used.
Did you start using alcohol or drugs after problems in school began? (Required)
CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Did you ever need extra help in school? (Required)
CLICK IN the Yes or No radio button.
If Yes, select the answer that best describes the client’s response.
- English as a Second Language
- Special Education
- Speech Therapy
- Mobility Aid
- Behavioral Health Services
- Alternative School
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
What area of school caused you the most problems? (Required)
CLICK ON the answer that best describes the client’s response.
- Math
- Language
- Arts
- Physical Education
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Have you gotten so high or sick from alcohol or drugs that it kept you from fulfilling work or school obligations? (Required)
- CLICK IN the Yes or No radio button.
NOTE: Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Have you spent less time at work or school so that you could drink or use drugs? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. The answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
In the last 12 months have you been bullied? (Required)
- CLICK IN the Yes or No radio button.
Are you currently in school? (Required)
- CLICK IN the Yes, No, or N/A radio button.
Would you like assistance with your educational status? (Required)
- CLICK IN the Yes or No radio button.
Would you like assistance with obtaining a GED? (Required)
- CLICK IN the Yes or No radio button.
Comments (Optional)
- Add comments related to staff information in the text box.
- CLICK IN the text box and TYPE IN the information.
Employment Section
Are you currently employed? (Required)
- CLICK IN the Yes, No, or N/A radio button.
What is your employment status? (Required)
- Document the client’s employment status at the time of admission.
- CLICK ON one of the items in the dropdown list.
|
Full time |
36-40 hours per week including active duty members of the uniformed services |
|
Part time |
1-35 hours a week |
|
Unemployed |
0 hours a week; Looking for work during the past 30 days or on layoff from employment |
|
Not in Labor Force |
Not looking for work during the past 30 days or a student, homemaker, disabled, retired or an inmate of an institution. |
|
Unknown |
Client doesn’t know how to answer this item |
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
Reason Not in Labor Force? (Required)
This item only displays if the answer is “Not in Labor Force” to the question “What is your employment status?”
CLICK ON one of the following items in the dropdown list:
- Disabled
- Homemaker
- Inmate
- Retired
- Student
- Seasonal Worker
- Other
- Not Applicable
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
What is the longest time you have held a full-time job? (Required)
CLICK ON one of the following items in the dropdown list:
- N/A
- 30 days
- 180 days
- 1 year
- 2-4 years
- 5+ years
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
Would you like assistance with your employment status? (Required)
- CLICK IN the Yes or No radio button.
What is your primary source of income? (Required)
Document the client’s primary source of financial support.
For children under 18, document the parents’ primary source of income or financial support.
CLICK ON one of the items in the dropdown list:
- Disability
- Public Assistance
- Retirement/pension
- Wages/Salary
- Other
- None
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
Have you ever received income from SSI? (Required)
- CLICK IN the Yes, No, or N/A radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
When you work, what type of work do you do? (Required)
- CLICK IN the text box and TYPE IN the information.
Have you ever engaged in illegal activities for profit? (Optional)
- CLICK IN the Yes or No radio button.
If yes, please explain. (Optional)
- CLICK IN the text box and TYPE IN the information.
Are you currently active duty in the United States military? (Required)
- This question displays for adults only.
- CLICK IN the Yes or No radio button.
Have you ever served in the military? (Required)
- This question displays for adults only.
- CLICK IN the Yes, No, or N/A radio button.
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
Did you serve in the National Guard, Reserves, Coast Guard or in any of the Active Duty Services? (Optional)
- This is a question that displays for adult clients only.
- CLICK IN the Yes or No radio button.
If you served in the military what was the discharge status on your Defense Department Form 214? (Required)
This question displays for adults only.
This item will display only if the answer is yes to “Have you ever served in the military?”
CLICK ON one of the items in the dropdown list:
- Medical
- Honorable
- Other than Honorable
- Unknown
Would you like assistance with your Veterans Affairs Services? (Optional)
- This field displays for adults only.
- CLICK IN the Yes or No radio button.
Comments (Optional)
Add text to document additional information the client shared about education or employment that is relevant to requested services.
CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
This Date represents the date of the document Status.
Legal Tab
Historical Legal Information
- Document the client’s past legal history and current legal status.
When you were growing up, did any of your household members go to prison? (Required)
CLICK IN the Yes or No radio button
If Yes, whom: CLICK ON one of the items in the dropdown list:
- Mother
- Father
- Stepparent
- Sibling
- Grandparent
- In Home Relative
- Non-Relative in Home
- Foster Parent
NOTE: This question is from the ACE Questionnaire. The ACE Questionnaire contains Adverse Childhood Experiences (ACEs) which are potentially traumatic events that can have negative, lasting effects on health and well-being.
Were you ever in trouble with the law? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Were you ever arrested? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Past legal status? (Required)
CLICK ON one of the items in the dropdown list:
- Past Probation
- Past Parole
- Past Incarceration
- N/A
Comments (Optional)
- Add text to document additional information the client shared about legal experiences that are relevant to requested services.
- CLICK IN the text box and TYPE IN the information.
Current Legal Information
What is your current legal status? (Required)
CLICK ON one of the items in the dropdown list.
The options in the dropdown list are:
- Jail or Prison
- Probation
- Parole
- Diversion Program
- Awaiting Trial
- Awaiting Sentencing
- NA
In the past 30 days, how many times have you been arrested? (Required)
- TYPE a number in the available text box.
- A maximum of two characters are permitted.
- If the client had more than 96 arrests in the last 30 days, TYPE 96 in the text box and provide additional information in the Comments text box.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Would you like assistance with your legal status? (Required)
- CLICK IN the Yes or No radio button.
Who is your point of contact for Legal issues? (Required)
- TYPE the name of the person with whom the client is working to resolve legal issues. There is only enough space for a name.
- Additional contact information may be documented in the Comments text box below or on the General tab in the Current Service Provider section.
- CLICK IN the text box and TYPE IN the information.
Comments (Optional)
- Enter any additional information about the client’s legal issues that are relevant to requested services.
- CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
This Date represents the date of the document Status.
Physical Health Tab
Document answers to general questions about the client’s health, medical questions specifically related to substance use disorder symptoms, and potential co-occurring medical conditions that may increase the severity and consequences of substance use.
General/Historical Health
In the past 12 months:
Do you have a history of medical conditions or medical problems? (Required)
- CLICK IN the Yes or No radio button.
Have you used larger amounts of alcohol or drugs or used them for a longer time than you planned? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. This answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you tried to cut down on alcohol and drugs and were unable to do it? (Required)
- CLICK IN the Yes or No rdio button.
NOTE: This answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. This answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you gotten so high or sick from alcohol or drugs that it caused an accident or became a danger to you or others? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. This answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you gotten so high or sick from alcohol or drugs that it caused physical health or medical problems? Required)
- CLICK IN the Yes or No radio button.
Have you increased the amount of alcohol or drugs you were taking so that you could get the same effects as before? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. This answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you gotten sick or had withdrawals when you quit drinking or missed taking a drug?
- CLICK IN the Yes or No radio button.
NOTE: This answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. This answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you continued to drink or take drugs to avoid withdrawals or to keep from getting sick?
- CLICK IN the Yes or No radio button.
NOTE: This answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. This answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Has your physical health been so bad that it resulted in hospitalization?
- CLICK IN the Yes or No radio button.
Comments (Optional)
- Type in the available text box any additional information obtained during the interview with the client that relates to physical health issues relevant to the delivery of services.
- CLICK IN the text box and TYPE IN the information.
Current Health
Do you currently have a chronic medical condition? (Required)
CLICK IN the Yes or No radio button.
- If yes, explain.
- The system displays this question when the answer is yes to “Do you currently have a chronic medical condition?”
- Type in the available text box clear and concise information about the client’s chronic health issues that may impact the client’s needs and response to services.
Are you currently taking any prescribed medications for medical reasons? (Required)
- Document any medications the client is prescribed by a medical professional whether they are currently taking the medications or not.
- CLICK IN the Yes or No radio button.
If yes, what are they? (Conditionally Required)
- The system displays this question when the answer is yes to “Are you currently taking any prescribed medications?”
- TYPE IN the available text box clear and concise information about the client’s medications.
Are you enrolled in Medication Assisted Treatment? (Required)
- CLICK IN the Yes or No radio button.
NOTE: Answering “Yes” to this item will result in this field displaying on the client’s CMBHS Treatment Plan.
Are you prescribed any of the following? (Conditionally Required)
This field will only display if the answer to “Are you enrolled in Medication Assisted Treatment?” is “Yes”.
CLICK ON one of the items in the dropdown list:
- Naloxone
- Suboxone
- Methadone
- Subutex
- Buprenorphine
- Vivitrol
Have you recently stopped prescription use of Vivitrol (naltrexone), methadone, or buprenorphine (Suboxone, Subutex)? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer to this item is used in the HHSC Priority Population calculation.
Have you experienced a non-fatal overdose? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer to this item is used in the HHSC Priority Population calculation.
If “yes” then, have you ever been administered naloxone or Narcan? (Conditionally Required)
- This question displays when the answer is yes to “Have you experienced a non-fatal overdose?”
- CLICK IN the Yes or No radio button.
NOTE: The answer to this item is used in the HHSC Priority Population calculation.
In the past 30 days, how many days have you been hospitalized? (Required)
- Type a number in the available text box.
- Maximum characters are two.
- If the client had more than 96 hospitalizations in the last 30 days, Type 96 in the text box and provide additional information in the Comments text box.
Have you given birth in the past 18 months? (Required)
- CLICK IN the Yes or No radio button.
- This question and the next question display only when the client profile choices are “Female.”
If “yes” then, have you used opioids in the past 3 years? (Conditionally Required)
- This question displays when the answer is yes to “Have you given birth in the past 18 months?”
- CLICK IN the Yes or No radio button.
- The answer to this item is used in the Priority Population calculation.
Are you currently pregnant? (Conditionally Required if the client is female)
- This question and the next question display only when the client profile choices are “Female.”
- This field specifies whether the client was pregnant at the time of assessment.
- CLICK IN the Yes or No radio button.
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
Do you think you could be pregnant? (Conditionally Required)
- This item only displays if the answer is no to “Are you currently pregnant?”
- CLICK IN the Yes, No, or Unknown radio button.
Are you using tobacco? (Required)
- CLICK IN the Yes or No radio button.
Would you like assistance to cut back or quit? (Conditionally Required)
- This question is only displayed, and is required, if you answered Yes to “Are you using tobacco?”
- This field generates a tobacco cessation referral.
- CLICK IN the Yes or No radio button.
Do you have any allergies? (Required)
- CLICK IN the Yes or No radio button.
If yes, what are they? (Conditionally Required)
- This question is only displayed, and is required, if you answered Yes to “Do you have any allergies?”
- CLICK IN the text box and TYPE IN the information.
- TYPE IN the available text box clear and concise information about the client’s allergies that impact the client’s services.
Would you like assistance with: (Required)
CLICK IN the box next to each item representing a service for which the client would like to receive assistance.
These are areas of concern that can be entered on the Referral pages to assist the client’s course of treatment or discharge support.
- Physical health
- Dental health
- Vision care
- Medical Insurance
- Medical Prescription
- HIV Medical Care
- STD/STI Services
- HCV Services
- Prenatal Care
- Reproductive/Sexual Health
Comments (Optional)
TYPE IN the available text box any additional information obtained during the interview with the client that relates to physical health issues relevant to the delivery of services.
Document Status (Required)
Select the appropriate Document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
This Date represents the date of the document Status.
Mental Health Tab
Clinicians document information about the client’s mental health when the client is not under the influence of mind-altering substances. During the interview, clinicians need to ensure the client understands that the symptoms described on this tab represent things that happen when the client is not directly under the influence of mind altering substances. Historical and current information is documented in two separate sections.
Historical Mental Health Information
Did you receive childhood mental health services? (Required)
- CLICK IN the Yes, No, or Unknown radio button
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Other than a problem with substance use, have you been told you have mental health difficulties or disorders? (Conditionally Required)
- This field displays when the answer is yes to “Other than a problem with substance use, have you been told you have mental health difficulties or disorders?“
- CLICK IN the Yes or No radio button.
If yes, what were you told: (Conditionally Required)
- CLICK IN the text box and TYPE IN the information.
- The text box limit is 250 characters.
Was a household member depressed or mentally ill? (Optional)
- CLICK IN the Yes or No radio button.
Did a household member attempt suicide? (Required)
- This question screens for suicide risk factors.
- CLICK IN the Yes or No radio button.
NOTE: This question comes from the ACE Questionnaire.
Have you experienced changes in sleep, eating or your weight? (Optional)
- This question screens for suicide risk factors.
- CLICK IN the Yes or No radio button
Have you ever: Heard voices no one else could hear or seen objects or things which others could not see? (Optional)
- CLICK IN the Yes or No radio button
Have you ever: Felt that people had something against you, without them necessarily saying so, or that someone or some group may be trying to influence your thoughts or behavior? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you were so full of energy and your ideas came very rapidly? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you talked nearly non-stop? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you needed little sleep? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you experienced feelings of sadness that were unbearable? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you lost pleasure in all or almost all activities? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you felt worthless or had excessive or inappropriate guilt? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period: When you have been unable to make decisions, concentrate, or think? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you had trouble: Getting along with others without arguing or fighting? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Had difficulty managing anger? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Experienced excessive anxiety and worry? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Believed you could do almost anything? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Engaged in self-injurious behavior? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Tried to hurt or kill an animal? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Tried to hurt or kill a person? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had a period when you: Intentionally damaged property that was not yours? (Optional)
- CLICK IN the Yes or No radio button
How many times have you been treated for psychological problems in a hospital/residential treatment setting? (Required)
CLICK ON one of the options available that best matches the client’s answer.
- 0
- 1
- 2
- 3
- 4
- 5
- 6+
NOTE: The next question is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. The answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Has your use of alcohol or drugs caused emotional or psychological problems? (Optional)
- CLICK IN the Yes or No radio button.
Do you frequently have difficulties with any of the following?
NOTE: These questions are Life History Screening questions. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Do you frequently have difficulties Concentrating and paying attention? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties Understanding what adults are telling you? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties remembering things? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties following rules and instructions? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties getting along with others without arguing or fighting? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties being on time? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties keeping enough money to last you throughout the month? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently find yourself getting really upset at little things or what people have told you are little? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties concentrating and paying attention? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties understanding what adults were telling you? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulties getting along with others without arguing or fighting? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently have difficulty being on time? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently do things that later you wish you hadn’t done? (Optional)
- CLICK IN the Yes or No radio button
Do you frequently forget or miss appointments? (Optional)
- CLICK IN the Yes or No radio button
Are you frequently being surprised when you are in trouble? (Optional)
- CLICK IN the Yes or No radio button
Have you wished you were dead or wished you could go to sleep and not wake up? (Optional)
- CLICK IN the Yes or No radio button
Have you ever tried to commit suicide? (Required)
- This question screens for suicide risk factors.
- CLICK IN the Yes or No radio button
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Comments (Optional)
- This text field is for additional comments about the client’s mental health.
- CLICK IN the text box and TYPE IN the information.
Current Mental Health Information
Are you currently seeing a Licensed Professional of the Healing Arts (LPHA) for a mental health condition or problem? (Optional)
- Document in this field whether the client is receiving services from an LPHA for his or her alcohol or drug use.
- CLICK IN the Yes or No radio button.
If yes, what are you being treated for? (Conditionally Optional)
- CLICK IN the text box and TYPE IN the information.
If yes, are you taking any prescription medications? (Conditionally Optional)
- CLICK IN the text box and TYPE IN the information.
If yes, what are they? (Optional)
- CLICK IN the text box and TYPE IN the information.
Are you currently having thoughts of killing yourself? (Optional)
- This question screens for suicide risk factors.
- CLICK IN the Yes or No radio button
Would you like assistance with your mental health? (Optional)
- CLICK IN the Yes or No radio button
Comments (Optional)
- This text field is for additional mental health comments.
- CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
This Date represents the date of the document Status.
Family & Social Tab
Users document information about the client’s family, social and living environment in this tab.
Family History
Were you raised by someone other than your biological/birth parents? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
How many living situations (different primary caregiver) did you have while you were growing up? (Required)
- CLICK IN the text box and TYPE IN the information.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Did you live with anyone who was a problem drinker or alcoholic or who used street drugs? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question comes from the ACE Questionnaire.
Did a parent or other adult in the household often: (Required)
NOTE: These questions come from the ACE Questionnaire.
— Swear at you, insult you, put you down or humiliate you? (Required)
- CLICK IN the Yes or No radio button.
OR
— Act in a way that made you afraid that you might by physically hurt? (Required)
- CLICK IN the Yes or No radio button.
— Push, grab, slap, or throw something at you? (Required)
- CLICK IN the Yes or No radio button.
OR
— Ever hit you so hard that you had marks or were injured? (Required)
- CLICK IN the Yes or No radio button.
Did an adult or person at least 5 years older than you ever:
— Touch or fondle you or have you touch their body in a sexual way? (Required)
- CLICK IN the Yes or No radio button.
OR
— Attempt or actually have oral, anal or vaginal intercourse with you? (Required)
- CLICK IN the Yes or No radio button.
Did you often feel that:
NOTE: This section has questions that come from the ACE Questionnaire.
— No one in your family loved you or thought you were important or special? (Required)
- CLICK IN the Yes or No radio button.
OR
— Your family didn’t look out for each other, feel close to each other, or support each other? (Required)
- CLICK IN the Yes or No radio button.
— You didn’t have enough to eat, had to wear dirty clothes, and had no one to protect you? (Required)
- CLICK IN the Yes or No radio button.
OR
— Your parents were too drunk or high to take care of you or take you to the doctor if you needed it? (Required)
- CLICK IN the Yes or No radio button.
— Were your parents ever separated or divorced? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The following questions come from the ACE Questionnaire.
— Was your mother or stepmother often pushed, grabbed, slapped, or had something thrown at her? (Required)
- CLICK IN the Yes or No radio button.
OR
— Was your mother or stepmother sometimes or often kicked, bitten, hit with a fist, or hit with something hard? (Required)
- CLICK IN the Yes or No radio button.
OR
— Was your mother or stepmother ever repeatedly hit at least a few minutes or threatened with a gun or knife? (Required)
- CLICK IN the Yes or No radio button.
Comments (Optional)
This text field is for additional family history comments.
- CLICK IN the text box and TYPE IN the information.
Maternal Alcohol Use
To your knowledge, did your mother ever drink alcohol that caused problems for her or others around her? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Did your mother drink alcohol when you were young? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Did your mother drink alcohol while she was pregnant with you? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Has anyone ever said anything to you about your mother’s drinking during her pregnancy with you? (Required)
- CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
Comments (Optional)
- This text field is for additional maternal alcohol use comments.
- CLICK IN the text box and TYPE IN the information.
Living Situation
As an adult, have you ever lived on your own? (Required)
CLICK IN the Yes or No radio button.
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab.
How long have you lived on your own at any one time? (Required)
This question displays for adult clients only.
CLICK ON one of the options available:
- NA
- 3 months
- 6 months
- 1 year
- 2 years
- 3 years
- 5 years
- Over 5 years
Have you ever been homeless? (Optional)
- CLICK IN the Yes or No radio button
Have you ever been without any family, friends, or caretakers? (Optional)
- CLICK IN the Yes or No radio button
Have you ever had state protective services involved with your family? (Optional)
- CLICK IN the Yes or No radio button
— As a child? (Optional)
- CLICK IN the Yes or No radio button
— Since being an adult? (Optional)
- This question displays for adult clients only.
- CLICK IN the Yes or No radio button
Have you ever had a history of Intimate Partner Violence? (Optional)
- CLICK IN the Yes or No radio button
Have you ever been bullied at home? (Optional)
- This question screens for suicide risk factors.
- CLICK IN the Yes or No radio button
Comments (Optional)
- This text field is for additional trauma-related comments.
- CLICK IN the text box and TYPE IN the information.
Current Trauma
Do you currently feel safe where you live? (Required)
- This question displays for adult clients only.
- CLICK IN the Yes or No radio button
Do you currently feel safe with the people in your life? (Required)
- This question displays for adult clients only.
- CLICK IN the Yes or No radio button
Trauma Comments (Optional)
- This text field is for additional trauma-related comments.
- CLICK IN the text box and TYPE IN the information.
Current Social Status
What is your living situation? (Required)
This field contains the client’s living status including homeless, living with parents, in a supervised setting, living on his or her own, or in an unstable housing setting.
CLICK ON one of the options available:
- Dependent
- Independent
- Homeless
- Unstable Housing
NOTE: This question is a Life History Screening question. Answers to life history screening questions result in the display of options for modification to treatment on the Recommendation tab. See the full description of modification to treatment on the Recommendation Tab. This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
In the last 30 days have you been released from a secured environment such as residential substance use disorder treatment program, jail, or prison? (Required)
- CLICK IN the Yes or No radio button.
If “yes”, in the year before you entered the controlled environment did you use opioids? (Required)
- CLICK IN in the Yes or No radio button.
- The answer to this item is used in the Priority Population calculation.
Marital status: (Required)
Document the client’s marital status in this field.
- Divorced
- Never Married
- Now Married
- Separated
- Widowed
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
How many children do you have under the age of 18? (Required)
- CLICK IN the text box and TYPE IN the information.
- List your Children (Conditionally Required — this table displays only if the answer to “How many children do you have under the age of 18?” is more than 0.)
Child Name:
- CLICK IN the text box and TYPE IN the information.
Age:
CLICK IN the text box and TYPE IN the information.
Biological Sex:
CLICK ON one of the options available:
- Male
- Female
Legal Custody
CLICK ON one of the options available:
- Self
- Other Biological Parent
- Joint
- DFPS TIA, Foster
- TDCJ TIA, Detention
- Paternal Family
- Maternal Family
- Adoption Family
Are you currently working on reunification?
- CLICK IN the Yes or No radio button
Would you like assistance with reunification?
- CLICK IN the Yes or No radio button
Have you gotten so high or sick from alcohol or drugs that it kept you from fulfilling your family obligations? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. The answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you spent less time with your support system so that you could drink or use drugs? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. The answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Have you spent a lot of time getting alcohol or drugs, using them or recovering from their use? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. The answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
Has your use of alcohol or drugs caused problems with your support system? (Required)
- CLICK IN the Yes or No radio button.
NOTE: The answer is used in the Severity Score calculation. Please see full description of the severity score calculation in the Diagnosis tab section. The answer is used in the Dimension Calculator for the ASAM Recommended Course of Treatment. Please see full description of the Dimension calculation in the Recommendation tab section.
In the past 30 days, how many times have you attended a self-help group? (e.g., AA, NA, etc.) (Required)
Document in this field the number of times the client has attended a self-help group in the 30 days preceding the date of admission to treatment services.
CLICK ON one of the options available:
- No attendance in the past month
- 1-3 times in the past month
- 4-7 times in the past month
- 8-15 times in the past month
- 16-30 times in the past month
- Some attendance in the past month, but frequency unknown
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
In the past 30 days, how many times have you attended a community support group? (Required)
Document in this field the number of times in the past 30 days the client has attended a community support group non-affiliated with substance use services.
CLICK ON one of the options available:
- No attendance in the past month
- 1-3 times in the past month
- 4-7 times in the past month
- 8-15 times in the past month
- 16-30 times in the past month
- Some attendance in the past month, but frequency unknown
Do you do anything for fun? (Optional)
- CLICK IN the Yes or No radio button
If yes, please explain. (Conditionally Optional)
- CLICK IN the text box and TYPE IN the information.
If the client answers No to “Do you do anything for fun?” answer the questions below. (Conditionally Optional)
Does anything stop you from doing the above? (Optional)
CLICK ON one of the options available:
- Physical Limitations
- Transportation
- Education/Employment
- Family
- Finances
- Substance Use
Do you have any spiritual practices? (Optional)
- CLICK IN the Yes or No radio button
- If yes, please explain.
- CLICK IN the text box and TYPE IN the information.
How many people do you trust? (Optional)
CLICK ON one of the options available:
- 0-2
- 3-5
- 5+
How many people do you rely upon? (Optional)
CLICK ON one of the options available:
- 0-2
- 3-5
- 5+
Do any of your close friends or family use alcohol or other drugs? (Optional)
- CLICK IN the Yes or No
Do you and/or your friends/family have access to naloxone or Narcan to reverse an overdose? (Optional)
- CLICK IN the Yes or No radio button.
In the last twelve months have you: (Optional)
CLICK ON one of the options available:
- Changed your friends
- Changed the type of clothing (gang colors, gang symbols, gang type clothing)
- Experienced school problems (truancy, lost interest, suspended, detention)
- Distanced yourself from your support system
- Been involved in criminal justice system
- Do you need any help with the following?
Comments (Optional)
- This text field is for additional living situation and family dynamic comments.
- CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
- This Date represents the date of the document Status.
SUD Assessment Substance Use Tab
Users document information about the client’s substance use in this tab.
High Risk Behaviors
- Document information about the client’s high-risk behaviors here.
Have you ever injected drugs?
- CLICK IN the Yes or No radio button
Have you ever shared injecting equipment?
- CLICK IN the Yes or No radio button
Have you ever shared equipment for snorting drugs?
- CLICK IN the Yes or No radio button
Have you ever had unprotected sex without condoms or latex barriers?
- CLICK IN the Yes or No radio button
Have you ever had unprotected sex with someone who injects drugs?
- CLICK IN the Yes or No radio button
Do you have tattoos or piercings?
- CLICK IN the Yes or No radio button
Have you had a persistent cough (longer than three months) and not visited a doctor? (Required)
- CLICK IN the Yes or No radio button
Have you been tested/screened for TB within the past year? (Required)
- CLICK IN the Yes or No radio button
Comments (Optional)
- This text field is to document additional high-risk behavior comments.
- CLICK IN the text box and TYPE IN the information.
Substance Use
Age at first use of any substances? (Required)
Enter the client's age when substances other than alcohol were first used.
Have you ever sought Substance Use Treatment before today? (Required)
- CLICK IN the Yes or No radio button
Treatment Services Received Table
Number of Episodes
Enter a number in the text box for the number of treatment episodes the client received of this type.
Treatment Services Received
CLICK ON one of the answer choices to document the type of treatment the client reports receiving.
After you have selected the number and type of treatment episode, CLICK ON the Add button.
- Residential Detoxification Services (ASAM Level 3.7 Withdrawal Management)
- Ambulatory Detoxification Services (ASAM Level 2 Withdrawal Management)
- Intensive Residential Services (ASAM Level 3.5 Clinically Managed – Intensity Residential Services)
- Supportive Residential Services (ASAM Level 3.1 Clinically Managed – Low Intensity Residential Services)
- Outpatient Services (ASAM Level 1 Outpatient Services)
- Outpatient Services (ASAM Level 2.1 Intensive Outpatient Services)
- Medically Assisted Treatment for substance use
Sum of number of prior treatment episodes
- CMBHS will total and display the sum of all the treatment episodes.
NOTE: This field contains a required element from the Treatment Episodes Data Set Minimum Data Set.
In the past when you stopped using, have you had any of the following:
Select as many as the client reports.
CLICK IN the box next to each item the client disclosed:
- Shakes/Tremors
- Blackouts
- Memory Lapses
- Cravings
- Vomiting
- Nausea
- Profuse sweating
- Seizures
- Delirium Tremors (DT)
- Anxiety
- Hallucinations (Visual, Tactile, Auditory)
- Headaches
Comments (Optional)
- This text field is for additional historical detoxification comments.
- CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
- This date represents the date of the document Status.
SUD Assessment Diagnosis Tab
Strengths and Limitations
Client's Strengths (Required)
- CLICK IN the text box and TYPE IN the information about the client’s strengths.
NOTE: The Texas Administrative Code 25, Part 1, Chapter 448, Subchapter H Rule 448.803 Assessment requires a description of client’s strengths and weaknesses as well as a comprehensive list of client’s problems, needs, and strengths for each assessment.
Client's Limitations (Required)
- CLICK IN the text box and TYPE IN the information about the client’s limitations that might impact treatment.
NOTE: The Texas Administrative Code 25, Part 1, Chapter 448, Subchapter H Rule 448.803 Assessment requires a description of client’s strengths and weaknesses as well as a comprehensive list of client’s problems, needs, and strengths for each assessment.
Severity Score for Diagnosis
- CLICK ON the Calculate button to calculate the Severity Score.
- The result of the calculation will display Mild, Moderate, Severe after the words Severity Score.
- The table below shows the calculation and the source of the scores.
|
Severity |
Scores used in the Calculator |
|
|
Mild |
2-4 symptoms/questions answered yes |
|
|
Moderate |
5-7 symptoms/questions answered yes |
|
|
Severe |
8+/questions answered yes |
|
|
Severity |
Scores used in the Calculator |
Answers |
|
Tab |
Questions |
Values |
|
Education Tab |
Have you gotten so high or sick from alcohol or drugs that it kept you from fulfilling work or school obligations? |
Answer: Yes = 1 No = 0 |
|
|
Have you spent less time at work or school so that you could drink or use drugs? |
Answer: Yes = 1 No = 0 |
|
Physical Tab |
Have you used larger amounts of alcohol or drugs or used them for a longer time than you planned? |
Answer: Yes = 1 No = 0 |
|
|
Have you tried to cut down on alcohol and drugs and were unable to do it? |
Answer: Yes = 1 No = 0 |
|
|
Have you gotten so high or sick from alcohol or drugs that it caused an accident or became a danger to you or others? |
Answer: Yes = 1 No = 0 |
|
|
Have you gotten so high or sick from alcohol or drugs that it caused physical health or medical problems? |
Answer: Yes = 1 No = 0 |
|
|
Have you increased the amount of alcohol or drugs you were taking so that you could get the same effects as before? |
Answer: Yes = 1 No = 0 |
|
|
Have you gotten sick or had withdrawals if you quit drinking or missed taking a drug? |
Answer: Yes = 1 No = 0 |
|
|
Have you continued to drink or take drugs to avoid withdrawals or to keep from getting sick? |
Answer: Yes = 1 No = 0 |
|
Mental Health Tab |
Has your use of alcohol or drugs caused emotional or psychological problems? |
Answer: Yes = 1 No = 0 |
|
Family and Social Tab |
Have you gotten so high or sick from alcohol or drugs that it kept you from fulfilling your family obligations? |
Answer: Yes = 1 No = 0 |
|
|
Have you spent less time with your support system so that you could drink or use drugs? |
Answer: Yes = 1 No = 0 |
|
|
Have you spent a lot of time getting alcohol or drugs, using them or recovering from their use? |
Answer: Yes = 1 No = 0 |
|
|
Has your use of alcohol or drugs caused problems with your support system? |
Answer: Yes = 1 No = 0 |
Diagnosis
The clinician may enter up to 18 Diagnoses in the Diagnosis rows.
Enter a minimum of 3 characters of a code and a minimum of 5 characters of a descriptor to search for a diagnosis.
The clinician must ensure that the diagnosis in the number one (1) slot is the diagnosis for which the client is being treated. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM V), the diagnosis being treated is referred to as the Principal Diagnosis.
The clinician may arrange the numbers next to each diagnosis line in the order of treatment services.
The calculated severity will display based only on the diagnostic-related questions throughout the assessment. The diagnostic-related questions can be found on the physical health, mental health, family and social, and substance use tabs. The system will rearrange the diagnoses, so they are displayed in the order the clinician selected when the clinician added the diagnoses.
After a diagnosis has been found and displays in the row and a justification has been selected, the clinician needs to CLICK ON the Add button to add a diagnosis or diagnoses.
Order of Treatment Services Table
The search method for the diagnosis allows the clinician to type in three characters associated with the code or five characters associated with the diagnosis description, and the system will display all the codes related to the information typed in the row.
The clinician needs to CLICK ON the code that represents the diagnosis supported by the symptoms discovered during the assessment which match the criteria in the DSM V.
Diagnostic Justification (Optional)
CLICK ON the option that describes the reason the diagnosis was selected.
- By client report
- By clinician observation
- By collateral report
- By history
- By impression
- By physician report
Comments (Optional)
- This text field is for additional diagnostic comments.
- CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document Status and Save.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
- This date represents the date of the Document Status.
- It can’t be edited by the user.
Recommendations Tab
This tab displays the results of three calculations: the HHSC Priority Population Status, the ASAM Recommended Course of Treatment, and the HHSC SUD Levels of Care in the service array. A list of domains where the client may need assistance is also extracted from the assessment answers.
HHSC Priority Population Status
The HHSC Priority Population Status is calculated and displayed by CMBHS.
The Priority Population Status is View Only.
These are the Priority Populations:
- Pregnant Injecting Drug User
- Pregnant Substance User
- Injecting Drug User
- High Risk for Overdose
- Referred by DFPS
- Experiencing homelessness or housing instability
- Priority Population Designation Not Met
The following table has detailed information about how the HHSC Priority Population is calculated.
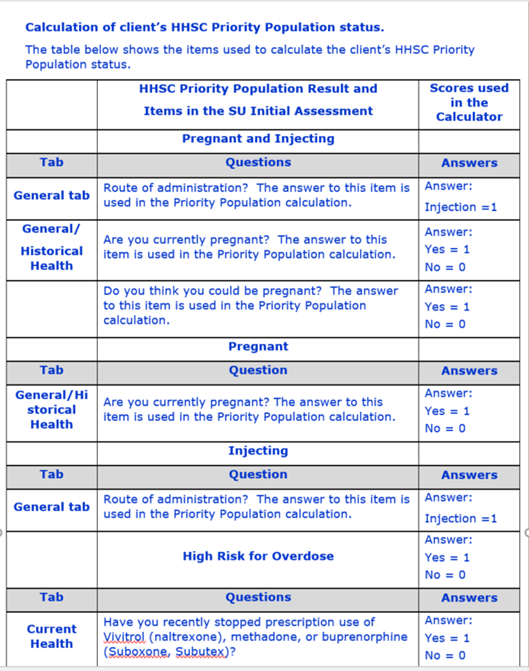
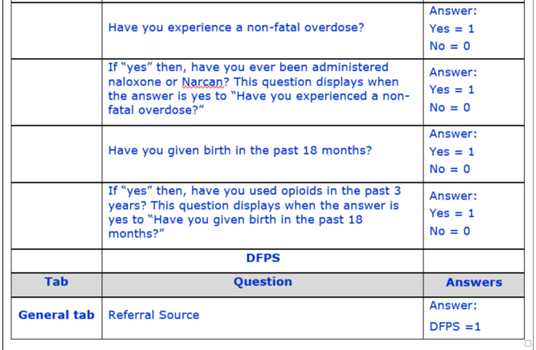
American Society of Addiction Medicine (ASAM) Dimensions
- Dimension 1: Acute Intoxication and/or Withdrawal Potential
- Dimension 2: Biomedical Conditions and Complications
- Dimension 3: Emotional, Behavioral, or Cognitive Conditions and Complications
- Dimension 4: Readiness to Change
- Dimension 5: Relapse, Continued Use, or Continued Problem Potential
- Dimension 6: Recovery /Living Environment
ASAM Recommended Course of Treatment
The array of services displayed in the ASAM Recommended Course of Treatment are a result of several factors obtained from questions in the assessment.
The reference to residential services includes both intensive and support residential services shown in the service array offered by SU contractors.
When a client declares there are no substances sought on the General tab, then there will be no ASAM recommended course of treatment.
The possible services listed in the order of treatment services are:
- Residential Detoxification
- Ambulatory Detoxification
- Residential
- Outpatient Services
- Medication Assisted Treatment
- Recovery Support Services
The Recommended Course of Treatment is calculated only in an Initial SU Assessment. The four calculations occur only in the Initial SU Assessment and do not occur in any subsequent assessment.
The ASAM Recommended Course of Treatment is a View Only field that displays CMBHS calculated results.
Determining the Course of Treatment
The method of determining the course of treatment includes the following elements in the calculation: Diagnosis + Severity + Dimension Score + Medication Assisted Treatment = Recommended Course of Treatment. The Severity component is a calculated field also based upon responses to items in the SU assessment. (See the table in the the Diagnosis Tab section.)
The Dimension component is a sum of the answers to questions that are grouped in the ASAM Dimensions. The assumption for establishing values for the answers to the dimension questions was based upon the risk of the client leaving services — the lower the number the less likely the person would leave services. The higher the number the more likely the client would stay in services. The sum of those scores indicates the volume of symptoms contained in the assessment resulting in a higher need for services.
A person with an Opioid Disorder not receiving Medication Assisted Treatment (MAT) is considered higher risk when the volume of symptoms is between 50 and 63.
The following table shows the questions associated with the ASAM Dimensions. The sum of the points assigned to the answers are used in the calculation for the ASAM Recommendation Course of Treatment.
Recommended Course of Treatment
The Recommended Course of Treatment is calculated only in an Initial SU Assessment. When a client declares there are no substances sought on the General tab, no ASAM recommended course of treatment will occur.
The four calculations occur only in the Initial SU Assessment and do not occur in any subsequent assessment.
The following table shows the questions associated with the ASAM Dimensions. The sum of the points assigned to the answers are used in the calculation for the ASAM Recommended Course of Treatment.
The Levels of Care in the HHSC SUD service array are:
- Residential Detoxification
- Intensive Residential
- Supportive Residential
- Outpatient Services
- Medication Assisted Treatment
- Ambulatory Detoxification
- Recovery Support Services
|
Tab |
Question |
Answer |
|
Dimension 1: Acute Intoxication and/or Withdrawal Potential |
||
|
Physical Health |
Do you have a chronic medical condition? |
Yes, No |
|
Substance Use |
In the past when you stopped using, have you had any of the following: |
Shakes/Tremors |
|
Dimension 2: Biomedical Conditions and Complications |
||
|
Physical Health |
Do you have a history of medical conditions or medical problems? |
Yes, No |
|
Physical Health |
Do you have a chronic medical condition? |
Yes, No |
|
Physical Health |
Are you currently taking any prescribed medications for medical reasons? |
Yes, No |
|
Physical Health |
Has your physical health been so bad that it resulted in hospitalization? |
Yes, No |
|
Physical Health |
Are you currently pregnant? |
Yes, No |
|
Physical Health |
Do you think you could be pregnant? |
Yes, No, Unknown |
|
Dimension 3: Emotional, Behavioral, or Cognitive Conditions and Complications |
||
|
Physical Health |
Are you enrolled in Medication Assisted Treatment? |
Yes, No |
|
Mental Health |
Historical Information section
|
Any Question answered "Yes" OR "Psychological Treatment Setting" field answer not zero |
|
Mental Health |
Are you currently seeing a Licensed Professional of the Healing Arts for any mental health condition or problem? |
Yes, No |
|
Mental Health |
If yes, are you taking any prescription medications? |
Yes, No |
|
Mental Health |
Are you currently having thoughts of killing yourself? |
Yes, No |
|
Mental Health |
Would you like assistance with your mental health? |
Yes, No |
|
Dimension 4: Readiness to Change |
||
|
General |
What Substances have you been using? (Primary) |
None, Not None |
|
Family Social |
In the past 30 days, how many times have you attended self‐help groups? (e. g., AA, NA, etc.) |
No attendance in the past month 1‐3 times in the past month 4‐7 times in the past month 8‐15 times in the past month 16‐30 times in the past month Some attendance in the past month, but frequency unknown |
|
Substance Use |
Have you ever sought Substance Use Treatment before today? |
Yes, No |
|
Dimension 5: Relapse, Continued Use, or Continued Problem Potential |
||
|
Physical Health |
Have you used larger amounts of alcohol or drugs or used them for a longer time than you planned? |
Yes, No |
|
Physical Health |
Have you tried to cut down on alcohol and drugs and were unable to do it? |
Yes, No |
|
Physical Health |
Have you gotten so high or sick from alcohol or drugs that it caused an accident or became a danger to you or others? |
Yes, No |
|
Physical Health |
Have you increased the amount of alcohol or drugs you were taking so that you could get the same effects as before? |
Yes, No |
|
Physical Health |
Have you gotten sick or had withdrawals when you quit drinking or missed taking a drug? |
Yes, No |
|
Physical Health |
Have you continued to drink or take drugs to avoid withdrawals or to keep from getting sick? |
Yes, No |
|
Family Social |
Have you spent a lot of time getting alcohol or drugs, using them or recovering from their use? |
Yes, No |
|
Dimension 6: Recovery /Living Environment |
||
|
General |
Referred by |
Community Health Service; Community Mental Health Services; Court Services/DWI/DUI; Department of Family Protective Services (Adult or Child Protective Services); Drug Court; Family/Friend; Hospital (Community); Hospital (State); Insurance/Employee Assistance Program; Outreach, Screening, Assessment, and Referral (OSAR); Peer Support/Recovery Support; Probation/Parole; School; Self (Client); Substance Use Disorder Prevention/Intervention/ Treatment; Work/Employer; Community Service Provider (local, state, federal) |
|
Education & Employment |
Have you gotten so high or sick from alcohol or drugs that it kept you from fulfilling work or school obligations? |
Yes, No |
|
Education & Employment |
Have you spent less time at work or school so that you could drink or use drugs? |
Yes, No |
|
Legal |
What is your current legal status? |
None Selected |
|
Family Social |
What is your living situation? |
Dependent |
|
Family Social |
Marital status: |
Divorced |
|
Family Social |
Have you gotten so high or sick from alcohol or drugs that it kept you from fulfilling your family obligations? |
Yes, No |
|
Family Social |
Has your use of alcohol or drugs caused problems with your support system? |
Yes, No |
|
Family Social |
Have you spent a lot of time getting alcohol or drugs, using them or recovering from their use? |
Yes, No |
|
Recommendation |
Client Support Needs |
Language or Auditory; Veterans Affairs; Education/ |
Key Life History Domains Modification to Treatment Recommended
The Life History Screening displays when the client needs modifications to treatment based on adverse life-course outcomes typically found in Fetal Alcohol Syndrome Disorder. The descriptions of modifications to treatment provide guidance for treatment planning.
How Key Life History Domains Modifications to Treatment
are Calculated
Key Life History Domains Modification to Treatment
The calculation first determines if there are answers in the three Key Life History Domains to indicate if the client is eligible for modifications to treatment.
If the client has three Key Life History Domains, then the Other Life History Domains are counted to determine if the client needs modifications to treatment.
If the client does not have three elements from the Key Life History Domains or the Other Life History Domains, the client does not need modification to treatment.
The Life History Screening includes the following questions:
Childhood History (Key Life Domain)
Were you raised by someone other than your biological parents?
Select Yes or No
Yes, results in inclusion to the calculation.
How many living situations (different primary caregivers) did you have while you were growing up (up to the age of 18) [Different people raising you].
More than 2 living situations results in inclusion to the calculation.
Maternal Alcohol Use (Key Life Domain)
To your knowledge, did your mother ever drink alcohol that caused problems for her or others around her?
Yes results in inclusion to the calculation.
Did she drink alcohol when you were young?
Yes, results in inclusion to the calculation.
Did your mother drink alcohol while she was pregnant with you?
Yes, results in inclusion to the calculation.
Has anyone ever said anything to you about your mother’s drinking during her pregnancy with you?
Yes results in inclusion to the calculation.
Education (Other Life History Domain)
What is the highest grade in school you completed?
10th grade or lower results in inclusion to the calculation.
Did you ever need extra help in school?
Yes, results in inclusion to the calculation.
What was the subject in school that caused you the most problems?
Math generates a result in inclusion to the calculation.
In what grade (or at what age) did you start using alcohol or drugs?
Before the age 12 results in inclusion to the calculation.
Criminal History (Other Life History Domain)
Were you ever in trouble with the law?
Yes, results in inclusion to the calculation.
Were you ever arrested?
Yes, results in inclusion to the calculation.
Employment and Income (Other Life History Domain)
What is the longest time the client has held a full-time job?
When the response is less than one year, it results in inclusion to the calculation.
Have you ever received SSI??
Yes, results in inclusion to the calculation.
Living Situation (Other Life History Domain)
As an adult, have you ever lived on your own (paying your own rent, etc.)?
No results in inclusion to the calculation. For adolescents, the answer should be NA, and this will not be counted towards scoring.
How long have you lived on your own at any one time?
When the response is less than 1 year, it results in inclusion to the calculation.
Mental Health (Other Life History Domain)
Other than a problem with substance use, what kinds of mental health difficulties or disorders have you been told you have?
More than 1 disorder results in inclusion to the calculation.
Have you ever tried to commit suicide?
Yes, results in inclusion to the calculation.
Day-to-Day Behaviors (Key Life Domain)
Do you frequently have difficulties with any of the following?
There is a list of 11 items, if the client answers yes to 5 or more than it results in inclusion to the calculation.
Client Selected Support Needs
The Client Support Needs are items from within all of the SUD Assessment tabs.
The clinician needs to check the boxes associated with every item for which the client has requested assistance. The clinician may edit any item on the original tab.
The Trauma items in the list will display results of the Adverse Childhood Experiences (ACEs) calculation and will remain as view only.
CLICK IN the boxes for the Support Needs the client has identified.
Comments (Optional)
- This text field is for additional comments about the client’s support needs.
- CLICK IN the text box and TYPE IN the information.
Document Status (Required)
Select the appropriate Document status and Save.
If you are not certain that you have completed the SUD Assessment, select Draft status.
- Draft
- Ready for Review
- Closed Complete
- Closed Incomplete
Document Status Date (System Generated)
- This date represents the date of the document status.
Update SUD Assessment
- Completed when there is a significant change in the client’s clinical and/or life situation and as required by law or contract.
- For substance use disorder services, there is no requirement that an update assessment be completed on a regular basis.
- An initial assessment completed by your organization can be updated at any time within the same episode of care, regardless of how old it is.
- An expired assessment can still be updated up to 30 days after it expires.
Update Assessment: Substance Use Services
After you have documented the Initial Assessment of a client, an Update Assessment may be completed in CMBHS on a periodic basis as required by law and for clinical and payment reasons.
CMBHS sends messages to remind staff when updates are due. However, these requirements reflect only the minimum necessary for publicly funded substance use and mental health services. So consult your organization’s experts or other sources to determine when updates are due for a specific client.
Although only a subgroup of the Initial Assessment questions must be answered for an Update Assessment, it is the responsibility of the clinician completing the assessment to review all the questions and enter client information as clinically appropriate.
Before You Start an Update assessment
- The CMBHS user must be assigned a role that permits documentation of a client assessment. To view a listing of Page Rights and Roles in CMBHS, click here.
- Verify that you have the correct client’s record by checking the client’s name and at least one other identifier before you begin to document an Assessment Update.
Business Rules for Update Assessments
- The client must have an Initial Assessment in Closed Complete or Closed Incomplete Status for this episode of care before you can document an Update Assessment.
- You cannot Update an Initial Assessment that is in Draft or Ready for Review status using the Update function.
- More than one Update Assessment can be completed for a client during an Episode of Care.
How to Document an Update Assessment for Substance Use Disorder
To document an Update Assessment, you must be at the Client Workspace.
When you are at the Client Workspace, pick Assessment from the Client Services Toolbar on the left side of your screen. A menu will drop down with the Assessment Types displayed. CLICK on Update SUD to select it.
NOTE: If Update Assessment is not available in the dropdown list (grayed out), it means that the Update Assessment is not appropriate to your current situation because there is not a valid Initial or Update SUD Assessment in the client’s record for you to update.
When the Update Assessment opens, the type is displayed at the top left of the page. The assessment type displays according to your location and the assessment type you have selected. Make sure that Update Assessment is displayed at the top of the page.
- When creating an Update Assessment, some fields are pre-filled with data from the most recent valid assessment.
- You will also need to CLICK the Recalculate button on the Recommendation page.
- Just like in all other Assessments, all required fields with a red * asterisk must be completed.